Hidradenitis suppurativa (HS) is a chronic, relapsing inflammatory skin condition that primarily affects the axillary, submammary, genital, inguinal, and perianal areas. Patients with HS typically develop inflammatory nodules, abscesses, sinus tracts, fistulas, scars, and contractures.1,2 The global prevalence of HS is estimated to be between 0.4% and 1%. Among the Caucasian population, the female-to-male ratio is approximately 3:1.1,2 The Hurley classification system, widely used to assess the clinical severity of HS, defines stage 1 as transient abscesses without scarring or sinus tracts, stage 2 as recurrent abscesses with the formation of a single sinus tract, and stage 3 as multiple abscesses and fistulas accompanied by extensive scarring.3,4 Treatment options include topical antiseptics, local and systemic antibiotics, high-dose zinc therapy, intralesional and systemic corticosteroids, dapsone, cyclosporine A, retinoids and surgery. Biologic treatments with Adalimumab, Secukinumab and Bimekizumab provide promising non-surgical approaches for moderate to severe HS.2,5–8 Additionally, research into the use of other biologics and small molecules is ongoing.9–11 Nevertheless, a combination of systemic and surgical treatments remains the standard approach for patients with moderate to severe HS and may offer significant benefits. The pathogenesis of HS is still not fully understood, but it is believed to be multifactorial with a genetic predisposition. Mutations in three proteins of the γ-secretase complex are reported in these patients. Presenilins (PSEN), nicastrin (NCSTN), and presenilin enhancer 2 (PSENEN) are defective and absent, so the Notch signaling pathway is not activated. Such defection leads to epidermal hyperplasia, abnormal follicular keratinization, and cyst formation.12 HS is considered a systemic disease, being associated with type II diabetes mellitus, polycystic ovary syndrome (PCOS), metabolic syndrome, obesity, dyslipidemia, hypertension, inflammatory bowel disease, spondyloarthropathy, and psychiatric comorbidities such as depression. In this context, the link between HS and malignancy remains a subject of ongoing debate. However, there is insufficient evidence regarding the incidence of malignancies in patients with HS. Hence, this study seeks to integrate insights into the pathogenesis of HS with a review of the current evidence on the relationship between HS and malignancy.
Methods
Search Strategy
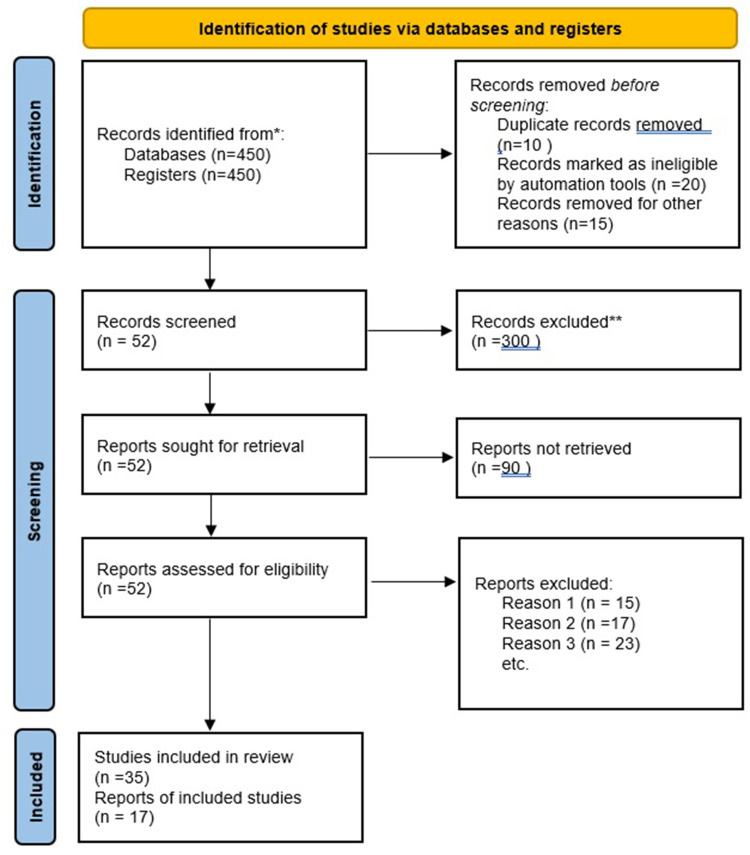
In this systematic review, we conducted a search across PubMed, Medline, and Web of Science in November 2024, adhering to the 2020 PRISMA guidelines.13 The search terms used were: (“hidradenitis suppurativa” OR “acne inversa”) AND (“malignant disease” OR “cancer” OR “carcinoma” OR “neoplasm” OR “neoplasia” OR “skin cancer” OR “melanoma” OR “leukemia” OR “AIDS-related cancers” OR “sarcoma” OR “tumors” OR “lymphoma” OR “metastases” OR “metastasis” OR “mycosis fungoides” OR “sezary-syndrome” OR “chemotherapy” OR “radiation” OR “immunotherapy” OR “tumor surgery” OR “hematological diseases” OR “overall cancer risk” OR “cancer incidence”). We identified 450 relevant articles published between 1978 and 2024; of these, only 52 had the inclusion criteria we had chosen. Figure 1 illustrates the flowchart of the search process.
Eligibility Criteria
Meta-analyses, experimental studies, case-control studies, cross-sectional studies, cohort studies, and recently published case reports and series were included if they were published in English and focused on human populations. Reviews, abstracts, and letters to the editor were excluded from this analysis. Two medical scientists independently screened and selected eligible articles, with a third scientist consulted in cases of uncertainty regarding inclusion or exclusion. Titles and abstracts were initially screened to determine eligibility, followed by a comprehensive review of the full texts to assess the level of evidence based on the study type.
Results
HS and Global Cancer Risk
HS is associated with several comorbidities such as metabolic syndrome, diabetes mellitus type II, PCOS, inflammatory bowel disease and increased risk of cardiovascular disease.14 This is due to the chronic inflammatory nature of the disease that mainly manifests itself on the skin, but whose altered mechanisms of the immune system are also expressed systemically. This observation can also be applied to other chronic inflammatory skin conditions and even more investigated than HS, such as psoriasis.15 The relationship between HS and cancer is still debated.These patients are considered to have a higher risk of malignancy than the general population. A 2001 study of the Swedish population estimated a 50% increase in cancer prevalence in a cohort of 2119 patients with HS compared to the general population.16 The same study established a statistically significant increased risk for non-melanoma skin cancer (NMSC), with standardized incidence ratio (SIR) 4.6, liver cancer (SIR 10.0) and buccal cancer (SIR 5.5).16 An increased incidence among HS patients had also been observed for other cancers, but not in a statistically significant way.16 A more recent Korean study compared a population of 22468 hS patients with 179,734 matched controls and established a higher risk of cancer occurrence among HS patients, with an adjusted hazard ratio (aHR) of 1.28. Specifically, the most involved malignancies were Hodgkin lymphoma (HL) (aHR 5.08), oral carcinoma (aHR 3.10), central nervous system cancer (aHR 2.40), and NMSC (aHR2.06).17 Cancer risk was increased in both HS patients aged <40 years (aHR 1.34) and those ≥40 years (aHR 1.26), while among women with HS there were no statistically significant differences with controls (aHR 1.16), unlike affected men who showed aHR 1.37.17
Certainly, a common risk factor between HS and cancer is recognized. Smoking is more frequent in HS than controls. Cigarette smoking, in fact, promotes the increase of Tumor Necrosis Factor α (TNFα) and other inflammatory cytokines implicated in the onset of HS and stimulates keratinocytes differentiation and growth through nicotinic receptors present in sweat glands, resulting in infundibular hyperkeratosis.18 On the other hand, smoking is widely recognized as one of the major risk factors for cancer occurrence in various body districts and is estimated to be responsible for one third of cancer deaths.19 Considering that tobacco smokers’ rate is higher among patients with HS,20 it is clear that this also affects from a malignancy perspective. The relationship between alcohol and HS is controversial. Although a study by Walter et al observes a slightly increased risk of HS recurrence among alcohol users in surgically treated HS patients, in the literature mostly alcoholism has no statistically significant impact on this condition.21 The role of diet toward HS is also under investigation. Poor dietary habits can induce increased body mass index, with obesity being a recognized risk factor for HS.21




Leave a Reply