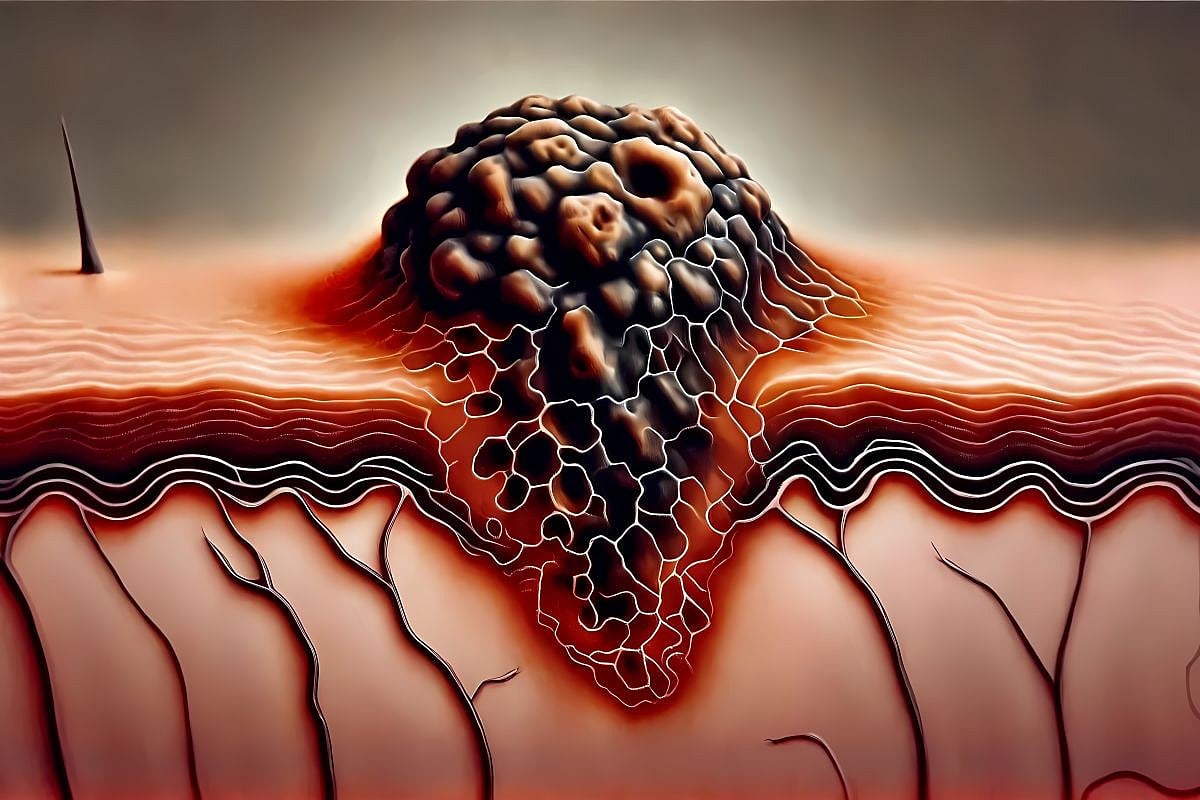
Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease characterized by painful nodules, abscesses, and sinus tracts, commonly referred to as tunnels [1]. These tunnels form due to chronic inflammation and repeated abscess formation, where ongoing tissue destruction creates interconnected subcutaneous tracts [2]. Typically emerging in advanced stages of HS, tunnels are critical indicators of disease severity and often necessitate surgical intervention, as they represent a chronic disease that is unresponsive to medical therapy alone [3,4]. Lined with granulation tissue or epithelium, tunnels are resistant to antibiotics and biologics, stressing the importance of complete surgical removal to prevent recurrence [5]. However, surgical planning requires a careful assessment, as excessive excision may lead to increased morbidity and impaired healing [6]. Accurately determining the tunnel length and extent is crucial for staging the disease, guiding surgical interventions, and optimizing outcomes [7].
Palpation, based on manual examinations, is commonly used in clinical settings to detect the presence and estimate the extent of tunnels in HS. While it is not a standardized or validated method for quantifying tunnel length, it remains a practical tool in routine dermatologic assessments. However, palpation is inherently subjective and may fail to detect deeper, branching, or subclinical tunnels. In contrast, high-frequency ultrasound (USG) has emerged as a promising imaging modality that enables the detailed visualization of dermal and subcutaneous structures [8]. USG can identify tunnel complexity and extent with greater precision, offering potential advantages for both diagnosis and surgical planning [9]. However, the comparative accuracy and reliability of USG and palpation in measuring tunnel lengths remain unexplored.
Despite the growing use of high-frequency ultrasound (USG) in dermatology, its specific application in measuring tunnel lengths in hidradenitis suppurativa (HS) remains underexplored. Palpation, though commonly used in clinical practice for tunnel detection, has notable limitations in identifying deeper or subclinical extensions. This highlights the need for more objective and reproducible assessment tools. Demonstrating the accuracy and reliability of USG in this context could enhance diagnostic precision and support more informed surgical planning. This study aims to evaluate the agreement between palpation and USG in preoperative tunnel length assessment in HS patients. By addressing this gap, the findings seek to support evidence-based refinements in clinical evaluation and inform future research on outcome-based utility.
2. Materials and Methods
2.1. Study Design and Setting
This study was a method comparison analysis conducted prospectively at an outpatient dermatology clinic, which serves as a referral center for the surgical management of HS. The primary aim was to evaluate the agreement between palpation and high-frequency USG in assessing tunnel lengths in patients undergoing surgery for HS. Secondary objectives included identifying lesion localization, determining disease severity through established staging systems, and examining the clinical characteristics of the study population.
2.2. Study Population
Patients diagnosed with HS who underwent the surgical excision of tunnels between May 2024 and August 2024 were included. Surgical decisions were guided by established practices, emphasizing wide excision as the preferred treatment modality for chronic and advanced stages of HS, particularly in cases unresponsive to medical therapy [10]. Wide excision was chosen where applicable to ensure the removal of irreversibly damaged tissue, including tunnels and scars, with the goal of optimizing disease control and minimizing recurrence risk. Eligible patients were those with a confirmed diagnosis of HS, persistent tunnels requiring surgical intervention, and complete preoperative data. Persistent tunnels were defined as non-healing lesions associated with recurrent symptoms or ongoing inflammation. Patients with incomplete medical records, coexisting dermatological conditions affecting subcutaneous tissue, or a history of surgery at the same site were excluded to ensure the accuracy of tunnel measurement and clinical outcomes.
2.3. Tunnel Length Measurement Methods
Tunnel length measurements were obtained preoperatively using palpation and high-frequency ultrasound with a 20 MHz linear probe. Palpation was conducted by two experienced dermatologists independently through a manual examination to estimate the extent of tunnels based on tactile feedback. Both dermatologists were blinded to each other’s measurements and to the USG results. Measurements were recorded in millimeters, and the average of the two dermatologists’ assessments was taken as the final value.
For USG imaging, if the tunnel’s start and end were visible in a single ultrasound image, measurements were taken directly using a digital caliper integrated into the device. When the tunnel could not be visualized in a single image, the ultrasound probe was positioned at a 90-degree angle to the skin surface, and the start and end points of the tunnel were marked on the skin. The distance between these points was then measured over the skin using a measuring tape. The USG identified the full extent of tunnels, including subclinical branches and surrounding inflammation. The final value for USG measurements was calculated as the average of the two dermatologists’ assessments, who were blinded to the palpation results.
2.4. Data Collection for Secondary Objectives
Demographic and clinical data were prospectively recorded to support the secondary objectives. Collected information included age, sex, body mass index (BMI), smoking status, and family history of HS. Disease severity was assessed using the Hurley staging system, which classifies HS into stages 1, 2, and 3 based on the presence and extent of abscesses, nodules, and tunnels [11]. Additional assessments included the International Hidradenitis Suppurativa Severity Score System (IHS4) and the Severity of Skin in Hidradenitis Suppurativa (SOS-HS) staging [12,13]. Treatment history, including the use of antibiotics, isotretinoin, and biologics like adalimumab, as well as treatment durations, was also documented. Lesion localization was categorized by the anatomical site, including axilla, inguinal, sacral, gluteal, areolar, perineal, pubic, and sternal regions.
2.5. Ethical Approval
Ethical approval was obtained from the Üsküdar University Non-Interventional Research Ethics Committee (date: 26 April 2024, no: 61351342/020-15). Written informed consent was obtained from all patients prior to their inclusion in the study. All data were anonymized to ensure confidentiality and compliance with ethical standards. This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki.
2.6. Sample Size
The sample size was calculated to require a minimum of 50 patients, based on recommendations for method comparison studies [14]. Additionally, considering the estimated prevalence of HS at approximately 0.7–1.2% in the general population, and that around one-third to one-half of patients present with moderate to severe disease (Hurley stage II/III) requiring surgical intervention, the recruitment of 50 patients was deemed both feasible and clinically representative [15,16]. Ultimately, 51 patients were enrolled in this study.
2.7. Analysis
The statistical analysis was conducted using Statistical Package for the Social Sciences (SPSS) version 30.0 (IBM Corp., Armonk, NY, USA) and MedCalc Statistical Software (version 20.104). Descriptive statistics for continuous variables were expressed as mean ± standard deviation (SD) or median (interquartile range [IQR]), and categorical variables were presented as frequencies and percentages. Normality was assessed using histograms. To assess inter-rater agreement between the two dermatologists performing palpation and USG measurements, the intraclass correlation coefficient (ICC) was calculated using a two-way random-effects model with absolute agreement. Both single and average measures of the ICC were reported to provide a comprehensive evaluation of agreement. The ICC analysis ensured the reliability of both methods and validated the consistency of the measurements obtained independently by the dermatologists. A combined approach using Bland–Altman and Passing–Bablok regression analyses was employed to ensure a robust evaluation of agreement and to identify systematic and proportional biases between measurement methods [17]. The agreement between palpation and USG measurements was evaluated using Bland–Altman and Passing–Bablok regression analyses. The Bland–Altman analysis was used to calculate the mean bias and limits of agreement (LoAs) to assess systematic differences and variability between the methods. LoAs were defined as the mean bias ± 1.96 standard deviations of the differences [18]. The assumption of a normal distribution for measurement differences was verified prior to performing the Bland–Altman analysis. Passing–Bablok regression was used to evaluate systematic and proportional biases between palpation and USG measurements. The intercept and slope were calculated, with a slope value including 1 within the 95% confidence interval (CI) indicating no proportional bias, and an intercept including 0 within the 95% CI suggesting no systematic bias [19]. The residual standard deviation (RSD) and ±1.96 RSD intervals were also reported to assess variability. The strength of the relationship between the two methods was determined using Spearman rank correlation. Statistical significance was defined as p < 0.05, and all statistical tests were two-tailed.




Leave a Reply