Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease characterized by painful papules, nodules, and abscesses as well as sinus tunnels and double-headed comedones (Del Duca et al, 2020; Diaz et al, 2023; Napolitano et al, 2017; Nguyen et al, 2021; Vossen et al, 2018). HS lesions primarily develop in intertriginous and apocrine gland–rich regions, such as the axillary, groin, perineal, perianal, and inframammary regions (Del Duca et al, 2020; Diaz et al, 2023; Napolitano et al, 2017; Nguyen et al, 2021; Vossen et al, 2018). The overall global prevalence of HS is estimated to be 0.40% (Jfri et al, 2021), with a prevalence of 0.7–1.2% estimated in the United States and Europe (Nguyen et al, 2021).
HS symptoms and associated pain can negatively impact QOL, psychosocial health, and physical function (McKenzie et al, 2020; Wolkenstein et al, 2007). HS is also associated with numerous comorbidities and inflammatory diseases that can further reduce health-related QOL, including depression, anxiety, cardiovascular disease, endocrine dysfunction, spondyloarthritis, and ulcerative colitis (Alotaibi, 2023; Cartron and Driscoll, 2019; Kimball et al, 2018; Machado et al, 2019; Nguyen et al, 2021; Thorlacius et al, 2018). Previous studies have demonstrated an association between HS and obesity, diabetes, and metabolic syndrome (Bui et al, 2018; Revuz et al, 2008; Rosi et al, 2021; Sabat et al, 2012). Pharmacological relationships underscore these epidemiologic observations (Lal and Herringshaw, 2024; Nicolau et al, 2024).
The time from onset of HS symptoms to diagnosis is reported to be 6–10 years, despite well-established diagnostic criteria (Garg et al, 2020; Kokolakis et al, 2020; Snyder et al, 2023). Patients with HS also reported an average of 5 physician visits and 5 misdiagnoses before receiving an HS diagnosis, highlighting the challenges in diagnosing this disease (Garg et al, 2020; Kokolakis et al, 2020). Although the exact reasons for delayed diagnosis are unclear, one contributing factor is thought to be a lack of awareness and understanding of HS pathophysiology among nondermatologic providers, with HS often misdiagnosed as infection, folliculitis, or boils (Snyder et al, 2023). Delays in HS diagnosis may lead to disease progression, irreversible scarring, impacts on psychosocial health, and reduced QOL for patients (Garg et al, 2020; Kokolakis et al, 2020; Snyder et al, 2023).
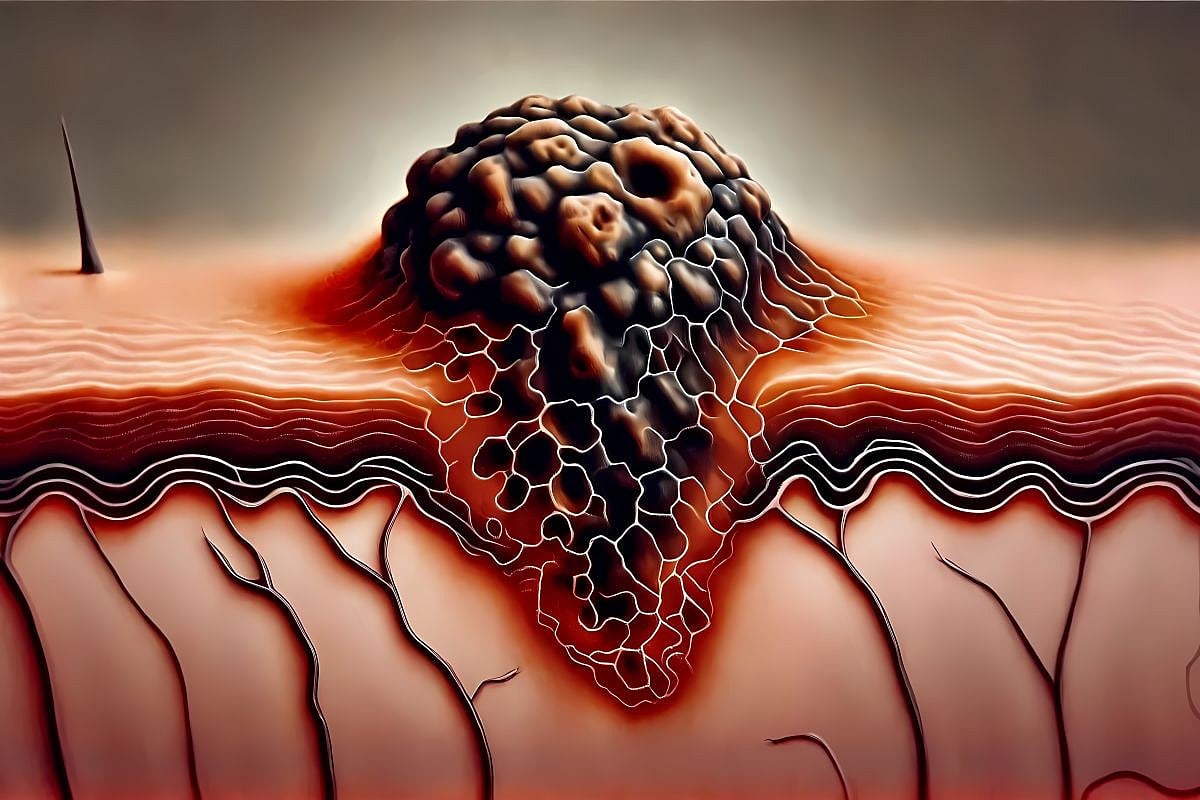
HS pathophysiology is driven by immune system dysregulation coupled with follicular inflammation and occlusion, largely due to genetic and environmental factors (Del Duca et al, 2020; Diaz et al, 2023; Napolitano et al, 2017; Nguyen et al, 2021; Rosi et al, 2021; Vossen et al, 2018). The abnormal inflammatory response underlying HS pathophysiology is mediated by neutrophils, monocytes, B and T lymphocytes, and numerous proinflammatory cytokines (such as TNF-α and IL-17), which causes chronic inflammation and skin lesions (Del Duca et al, 2020; Diaz et al, 2023; Napolitano et al, 2017; Nguyen et al, 2021; Vossen et al, 2018).
HS shares some pathogenic features of other inflammatory skin diseases, such as psoriasis, pyoderma gangrenosum, acne, folliculitis, pilonidal sinus disease (PSD), and alopecia areata (Figure 1). These diseases involve many of the same initiating events, inflammatory pathways, molecular and cellular features, and clinical features of HS. In addition, common comorbidities of HS (such as obesity, diabetes, and metabolic syndrome) are also associated with other inflammatory skin diseases (Al Ghazal et al, 2012; Bui et al, 2018; Kamiya et al, 2019; Laureano et al, 2014; Revuz et al, 2008; Rosi et al, 2021; Sabat et al, 2012; Villasante Fricke and Miteva, 2015; Winters and Mitchell, 2024). However, there are differences in inflammatory environments between HS and other inflammatory skin diseases, which leads to several distinguishing clinical characteristics of HS that are used in its diagnosis (Table 1). The overlap between HS and other inflammatory skin diseases highlights the heterogeneity and complexity of HS, which may explain why HS is sometimes misdiagnosed. In addition, the pathogenic similarities between HS and other inflammatory skin diseases present opportunities for repurposing disease management strategies, underscoring the need for physicians to fully understand which pathogenic factors are shared with other skin diseases and which are unique to HS.




Leave a Reply