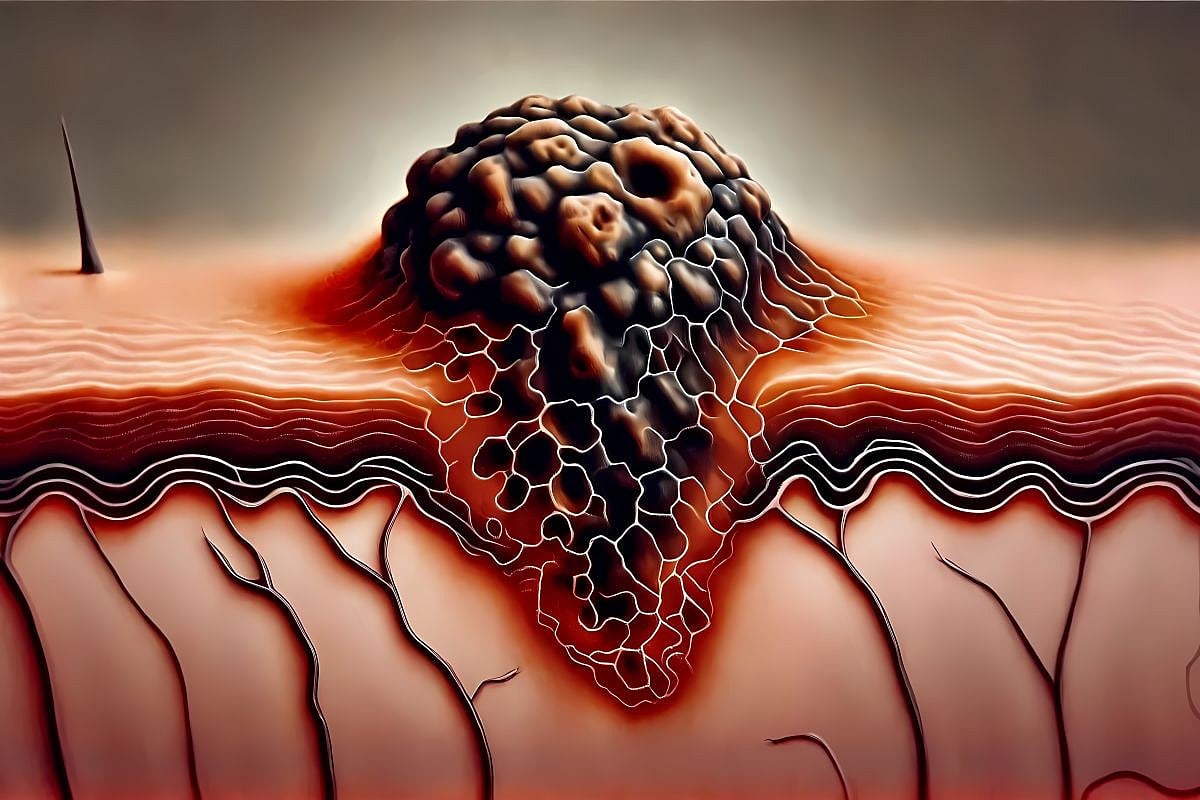
Hidradenitis suppurativa (HS) is a chronic inflammatory disease of the apocrine glands, characterized by recurrent episodes of improvement and exacerbation [1–2]. Lesions are typically painful, with the most commonly affected areas being the axillary, inguinal, and inframammary regions [1,3]. Clinical manifestations may include deep-seated nodules, abscesses, sinus tracts (skin tunnels), and fibrotic scarring [4–5].
The disease is more prevalent in women, with onset most commonly occurring between puberty and the age of 40. Diagnosis is primarily clinical, based on the characteristic presentation, involvement of typical anatomical locations, and recurrence of lesions [6]. In cases involving atypical lesion sites or initial presentations, dermatologic ultrasound can play a key role in supporting the diagnosis [5–6].
We present a case of HS in which ultrasonographic evaluation, in conjunction with other complementary examinations, helped confirm the diagnosis of HS in an atypical presentation site.
Case presentation
A 25-year-old male patient, originally from Brazil, reported recurrent infections in the cervical region for the past two years, necessitating the use of multiple antibiotics and drainage of secretions. The most recent recurrence occurred about one month before admission, with local progression of lesions in the cervical region. The patient did not present with fever or weight loss, denied any ongoing acute illness or trauma, and reported no current medications, prior incarceration, or contact with individuals with tuberculosis.
Upon clinical examination, the patient had two nodules in the cervical region, interconnected by a fistulous tract, with seropurulent content emerging from drainage orifices upon manual expression (Figure 1). Due to the patient’s country of origin and the history of multiple antibiotic treatments without resolution, the diagnostic hypothesis of skin tuberculosis (scrofuloderma) was considered.
Tests were requested, including polymerase chain reaction (PCR) with GeneXpert, tuberculin skin test (TST), chest X-ray, general laboratory tests, and serologies for hepatitis and HIV, to investigate tuberculosis and potential related comorbidities. A biopsy was also performed, with culture for fungi and bacteria from the seropurulent material collected from the patient’s clinical lesion. GeneXpert and TST presented negative results, and cultures showed no growth. The chest X-ray had no alterations, general laboratory tests were unremarkable, and serologies for hepatitis and HIV were non-reactive, ruling out infectious diseases.
A high-frequency dermatological ultrasound was performed to determine the extent of the lesion and assist in the diagnostic definition. The ultrasound revealed tortuous fistulous tracts in the dermis and subcutaneous, with hyperechoic fragments within (some linear, possibly corresponding to hair shafts and keratin), with increased vascularity observed on Doppler study connecting the mid-occipital region with the left posterior cervical region and the upper dorsal region of the midline, suggesting a case of HS (Figure 2).
Discussion
Atypical forms of HS are described in non-intertriginous areas where hair follicles are present [3–6]. The disease is characterized by nodules that can evolve into abscesses and the formation of fistulas. It is usually exacerbated by smoking and obesity and is correlated with a higher tendency to develop metabolic syndrome [7–8]. Despite the patient presenting clinical lesions suggestive of the disease, these were located in an atypical area, and he did not exhibit additional clinical stigmata associated with the condition.
Scrofuloderma is a subtype of cutaneous tuberculosis that progresses with the formation of nodules and fistulous tracts containing purulent material. The most common sites of involvement are the head and neck. It can evolve insidiously and may not respond to traditional antibiotic treatments [5,7]. Pulmonary involvement and elevated PPD are usually present. Clinical lesions manifested by scrofuloderma can mimic various skin diseases, making it necessary to rule out the diagnosis in areas with a high prevalence of this disease [9–10].
To assist with the differential diagnosis between scrofuloderma and HS, key clinical findings are summarized in Table 1 [11–12].
Thus, cutaneous tuberculosis in the form of scrofuloderma was initially the most relevant clinical hypothesis, as the patient was from a high-risk area for the disease and presented with clinical lesions characteristic of the disease in the most common sites, despite denying known contact with carriers.
Skin biopsy is usually not required to confirm the diagnosis of HS; however, in cases in which the diagnosis is uncertain, a biopsy can be used to exclude other causes such as pyoderma gangrenosum, lymphomas, and squamous cell carcinoma. Findings related to HS depend on the type of alteration in the biopsied area, which may show a cyst, nodule, or abscess in an inflamed sinus tract or a scar resembling a cord [6,8].
The use of high-frequency ultrasound in clinical research shows the occurrence of multiple retained hair follicles, confirming the role of hair follicles as foreign bodies that contribute to the perpetuation of inflammation in areas with HS. On ultrasound imaging, vellus hairs appear as bilaminar hyperechoic structures located between cysts or fistulas, oriented parallel to the skin surface, unlike unaffected hair follicles, which are oriented perpendicularly. In the patient, the ultrasound evaluation found a fistulous tract connecting the nodules interspersed with hair follicles [13–14].




Leave a Reply