Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition characterized by recurring inflammatory nodules, abscesses, and, subsequent to this, the occurrence of subcutaneous sinus tracts and scars1. It has a significant psychological and functional impact on patients due to the discomfort and odorous discharge from the lesions2. The global prevalence of HS is estimated to be 0.00033–4.1%, with a European-US population frequency of 0.7–1.2%3. The most common age of onset is between the ages of 20 and 40; however, new-onset HS has been documented in both younger and older individuals4,5. Because of poor mental health, lost employment, reduced intimacy, chronic pain, and substance use disorders, hidradenitis suppurativa has one of the most damaging effects on quality of life of any skin disorder6–9. These lesions appear in intertriginous regions and apocrine gland-rich areas, most often in the axillary, groin, perianal, perineal, and inframammary areas10. Multiple comorbidities, including metabolic syndrome, obesity, cardiovascular disease, chronic inflammatory bowel disease, and spondylarthritis, have been linked to HS11,12. Because of these issues, prompt diagnosis and efficient treatment are essential.
The pathophysiology of HS is still poorly understood. As a result, HS is a complicated condition with a difficult treatment. Although lifestyle changes, weight loss, quitting smoking, topical treatments, and oral antibiotics typically suffice for managing mild cases, dealing with moderate-to-severe hidradenitis suppurativa (HS), which often doesn’t respond well to traditional approaches, poses a significant challenge for healthcare professionals13.
This comprehensive review aims to offer valuable insights into the management of hidradenitis suppurativa (HS) by comparing assessment tools and treatment options. Our goal is to shed light on effective approaches that may benefit clinicians and researchers, thereby enhancing the care and understanding of this challenging condition.
Methodology
Using keywords like ‘hidradenitis suppurativa’, ‘acne inversa’, ‘diagnosis’, ‘treatment’, ‘surgery’, and ‘medication therapy’, studies were searched in databases including PubMed, PubMed Central, and Google Scholar. This review includes case reports, case series, reviews, observational studies, randomized control trials, and meta-analyses discussing hidradenitis suppurativa. Only studies that have been published in English are included in this review. One hundred eleven papers are included in this evaluation after the studies were thoroughly extracted and analyzed.
Pathophysiology
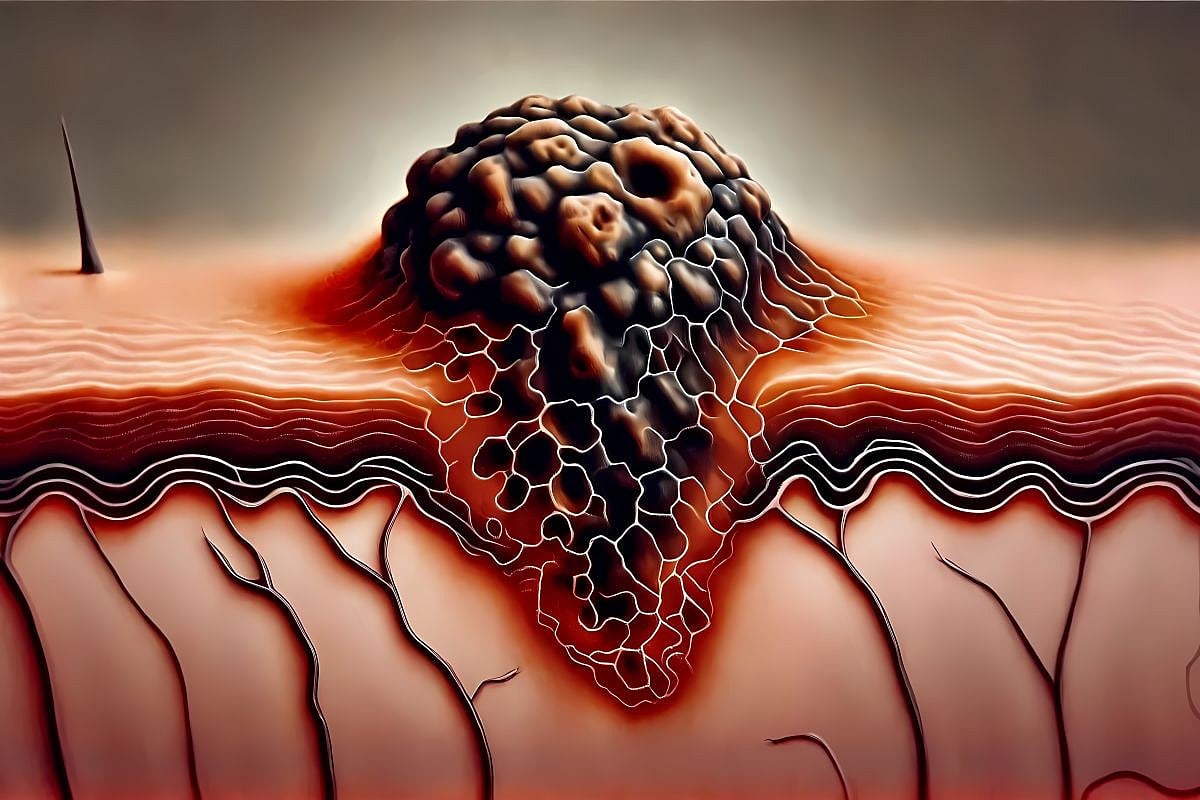
Although the etiology of HS is still unclear, significant advances have been achieved in recent studies3. In order to create effective treatments, it is imperative to further identify the various elements that contribute to HS. HS starts with follicular occlusion, which is likely due to infundibular keratosis and hyperplasia of the follicular epithelium, leading to the retention of secretions, rupture, and release of follicular contents14. Follicular content release in the dermis triggers an immune response that activates granulocytes, macrophages, plasma cells, and pro-inflammatory cytokines such as interleukins (IL-1, IL-17), tumor necrosis factor, and interferon, resulting in a vicious cycle of tissue destruction15. In later stages, this causes abscess formation, severe inflammation, sinus tract formation, and scarring5.
Multiple factors have been associated with HS, including lifestyle factors, genetic factors, and hormonal factors:
Lifestyle factors
Smoking, stress, and obesity are all lifestyle factors that contribute to the development of HS. A study discovered that people with HS were almost four times more likely to be smokers16. HS patients are also four times more likely to be obese than the general population, and BMI is positively correlated with disease burden17. It has also been suggested that psychological stress contributes to the onset and development of this illness. Stress can impair immune function, causing disease development or exacerbations18. Stress and worry can also lead to habits like smoking or binge eating, which can lead to the worsening of HS symptoms.
Genetic factors
In Western countries, HS normally appears as a sporadic form, but in 40% of cases, it arises as a family disorder19. Positive family histories are commonly reported by HS patients20, and autosomal dominant inheritance patterns in affected families have been identified21, which strongly suggests a genetic component to this condition. According to the genetic mutations linked to HS that have been discovered to date, HS can be inherited as a polygenic disorder brought on by abnormalities in genes controlling immune system function, ceramide synthesis, or epidermal proliferation, or as a monogenic trait caused by a defect in either the Notch signaling pathway or inflammasome function20. Chromosome 1p21.1–1q25.3 region has been linked to a mutation in the γ-secretase pathway in several families with HS patients20,22. These patients exhibit a severe phenotype of HS20. Mutations in the nicastrin (NCSTN) gene, presenilin 1 (PSEN 1), and presenilin enhancer (PSENEN) genes have all been linked to HS19,20,23–25.
Hormonal factors
Hormones are also considered a contributing factor in the pathogenesis of HS. Indicators of hormonal involvement include predominance in females, onset in puberty, and alterations in HS activity during times of changing hormones such as premenstrual periods, pregnancy, and menopause26. Activation of androgen receptors in the sebaceous gland causes increased sebum and inflammation, which can contribute to the blockage of hair follicles, ultimately leading to HS26. Although patients with HS have not been found to have greater than normal plasma levels of testosterone or 5-DHT, studies have shown that the use of anti-androgenic drugs has a beneficial response compared to antibiotic-based treatment alone26.




Leave a Reply