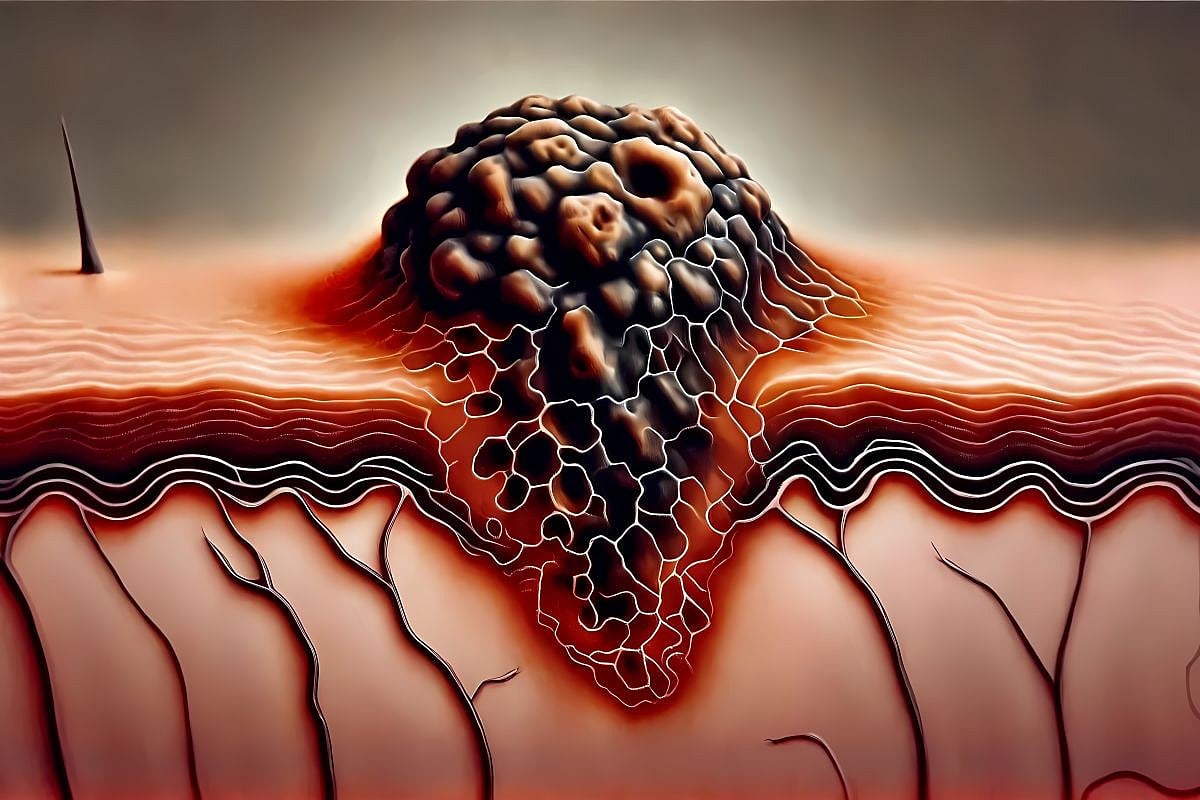
Hidradenitis suppurativa (HS), which is also known as acne inversus, is a skin disease characterized by chronic skin inflammation and skin lesions. The chronic inflammation caused by HS usually leads to the formation of skin lesions, nodules, abscesses, draining tracts, and fibrotic scars. 1 The skin lesions usually form in areas where there is frequent skin contact and tension or in areas with abundant apocrine glands. Thus, the most commonly affected areas in HS include the axillary, groin, perianal, perineal, and inframammary areas. 1
Over the few past years, various studies investigated the pathophysiology of HS, yet an exact cause is still not proven. It is hypothesized that both the environmental and genetic factors play a role in triggering the disease. On the environment side, cigarette smoking, obesity and overweight are prominent factors. Concurrently, the role of genetic factors has been displayed in many studies which showed 30%–40% of HS cases to have a family history of the disease. 2 HS pathophysiology starts with hair follicles occlusion and rupture, which leads to the release of keratin fibres into the dermis. An immune reaction is followed involving Neutrophil and lymphocytes recruited with the help from cytokines released from activated Macrophages which initiate the cascade necessary to start the innate immune upregulation and leukocyte attraction. Once both innate and adaptive immunity are dysregulated a clinical HS develops. Despite the fact that HS is not primarily an infectious disease, the rupture of pilosebaceous units and release of bacteria within the dermis leading to a local inflammatory response plays a critical role in HS pathophysiology by making the disease clinically worse and difficult to treat due to the diverse microbial profile of the colonies that will bind irreversibly to hair follicles and sinus tract epithelium leading to a sustained chronic inflammation. 1 , 2 HS symptoms, caused mainly by the skin lesions, include pain, bromhidrosis and scarring usually in highly innervated areas. 1 These symptoms adversely impact patient’s psychosocial health and general quality of life.
HS is one of the more common skin diseases, with an estimated global prevalence of 0.05%–4.1%. 3 Moreover, it has an estimated prevalence of 0.40% (95% confidence interval [CI] 0.26%–0.63%) reported in the United States, Australia, Scandinavian countries and Western European countries, 4 and this prevalence seems to only be increasing in the recent years. HS is a multifactorial disease where both genetic and environmental factors play a role in the pathogenic process of the disease. The rise in certain environmental factors might have caused the increased prevalence of HS in recent times. In this meta‐analysis, we intend to test and analyse the association of specific modifiable environmental risk factors. The modifiable risk factors we aim to explore are obesity, smoking status, type 2 diabetes mellitus (T2DM). We aim to establish a robust link between these risk factors and increased HS through quantitative meta‐analysis.
2. METHODS
2.1. Protocol and registration
This systematic review and meta‐analysis followed the preferred reporting items for systematic reviews and meta‐analyses (PRISMA) guideline. 5 The review protocol was registered in the international prospective register of systematic reviews (PROSPERO) online database with the identifier CRD42023486711.
2.2. Search strategy
For this systematic review and meta‐analysis, a search of academic databases including PubMed, Scopus, Embase, Web of Science, and cumulative index to nursing and allied health literature (CINAHL) Ultimate was conducted. The search strategy was first developed in PubMed and then transferred to the other databases using the Polyglot translator. 6 The predetermined search strategy for searching the databases used medical subject headings (MeSH) terms that included (‘Hidradenitis Suppurativa’ [MeSH] OR ‘obesity’ [MeSH] OR ‘body mass index’ [MeSH] OR ‘Diabetes Mellitus’ [MeSH]). The full search strategy can be found in the Supporting Information.
2.3. Eligibility criteria
Our inclusion criteria included original articles reporting either the odds ratio (OR) or the numbers of HS cases associated with obesity, smoking or T2DM. The selected studies were required to include a HS‐negative control group in an observational study design. No restrictions were imposed on the type of population, age or HS diagnostic criteria. Conversely, exclusion criteria comprised non‐original studies, specifically reviews, systematic reviews or meta‐analyses. Additionally, studies with duplicate datasets and those lacking a control group were excluded from our analysis.




Leave a Reply