Hidradenitis suppurativa (HS) is a chronic, relapsing inflammatory disease of the skin, characterized by recurrent draining sinuses and abscesses, predominantly in skin folds carrying terminal hairs and apocrine glands. Treatment for this debilitating disease has been medical management with antibiotics and immune modulators. With the advent of better reconstructive surgical techniques, the role of surgery in the treatment of HS has expanded, from being a last resort to a modality that is deployed earlier. Larger defects can be more easily reconstructed, allowing for a more radical excision of diseased areas. Locoregional flaps, perforator flaps, and propeller flaps that use the fasciocutaneous tissue allow reconstruction of defects with similar tissue, and provide better cosmetic and functional outcomes. They are easy to execute and can be performed even in resource-poor settings with concurrent use of immune modulators and postoperative antibiotics. Hidradenitis can be successfully treated with surgery in early stages as well as severe disease, due to the advances in understanding disease behavior, multidisciplinary care, and advanced reconstructive techniques. Coupled with a multidisciplinary care team, surgery offers a durable, lasting cure for HS, significantly reducing disease morbidity.
INTRODUCTION
Hidradenitis suppurativa (HS) is a long-ignored skin disease affecting 1% of young, underserved minorities globally: incidence is highest in African American people (1.3%), lowest in Hispanic/Latino people (0.07%), and intermediate amongst White people (0.75%),1 accounting for approximately 4% of the US population.2 Its cost impact on the patient (job losses/decreased work productivity and out-of-pocket costs) is high. Healthcare cost itself is estimated at more than $60,000 per year.3,4 Despite the prevalence, HS remains an orphan disease without proper diagnostic tools or established standard of care guidelines.
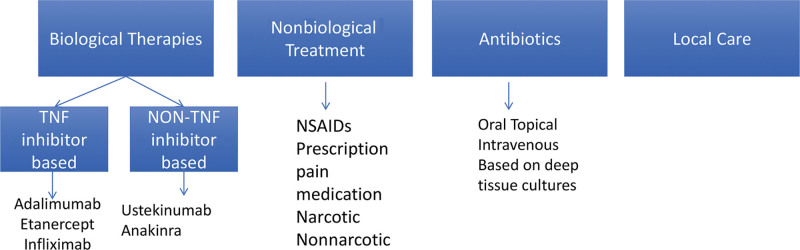
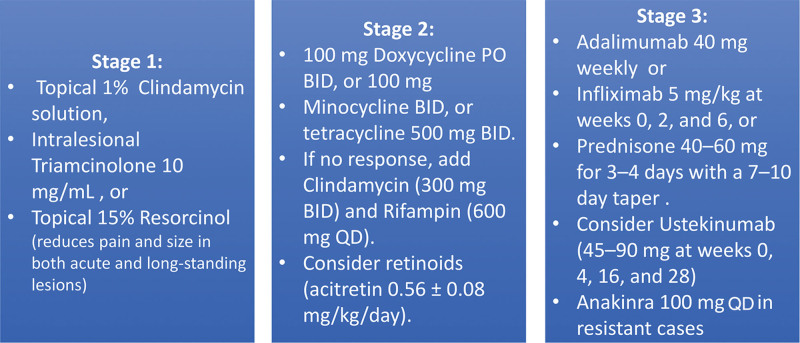
Primarily affecting hair follicles, HS quickly progresses to painful, severely debilitating complications.5 Traditionally, medical management is the first-line therapy (Fig. 1), and surgery, the “treatment of last resort” after a 3- to 6-month trial.6 Treatment recommendations based on Hurley stage (Fig. 2) have a strong bias that stems from the method by which treatment modalities have been comparatively studied: medical management (especially immunotherapy) of HS is better researched, whereas similar well-controlled studies in surgery are missing.
Surgical approaches include local destruction via cryosurgery, cryoinfusion, electrosurgery, and photodynamic therapy; incision and drainage; standard deroofing, wide deroofing, and debridement of individual sinus tracts; or complete surgical excision beyond all clinically apparent margins with reconstruction.7 That said, surgical treatment is based on anecdotal evidence, case studies, and case reports, with lower strength of recommendation scores8,9; clinical trials comparing the two approaches head-to-head, medical versus surgical, have never been performed. Recent cooperative reports have recognized these gaps and concluded that a thoughtful combination of surgical and medical treatments could potentially yield better results than using either of them alone.10,11
Here, we explore the expanding role surgery plays in the treatment of HS. Based on recent evidence, we posit that surgical extirpation and reconstruction, coupled with adjuvant antibiotic therapy, could offer a durable, long-lasting solution to a complex disease.
RATIONALE FOR SURGERY FOR HS
The reasoning for surgery to treat HS (arguably even better than medical strategies used alone) is rooted in novel characteristics of both HS as a disease and of HS patients in general.
- Disease Biology: The central pathogenic event in HS is the occlusion of the upper part of the hair follicle leading to perifollicular lympho-histiocytic inflammation.12 The structural alterations that follow (deep, invading abscess, multiple interconnecting sinus tracts, and deep communicating dermal and impregnable cicatrization) are barriers to any medical treatment. Antibiotics and immune modulators cannot easily penetrate this hostile microenvironment (scar tissue, acidic pH, aberrant vascularity), limiting their efficacy.13 In sharp contrast, surgery extirpates diseased tissue, reduces disease burden, and disrupts anatomic barriers (deroofing), making it a powerful adjunct to postoperative medical management.
- Staging: Clinical staging of HS (Hurley staging system; Fig. 2) demonstrates how early single lesions (stage I) are amenable to surgical excision and eradication of disease in one step, as opposed to long-term antibiotic care and flare-ups.14
- Recent surgical advances: Newer reconstructive techniques, elegant perforator flaps, biologics, sophisticated microsurgery, and the vacuum-assisted closure expand reconstructive choices and provide superior cosmetic and functional outcomes.
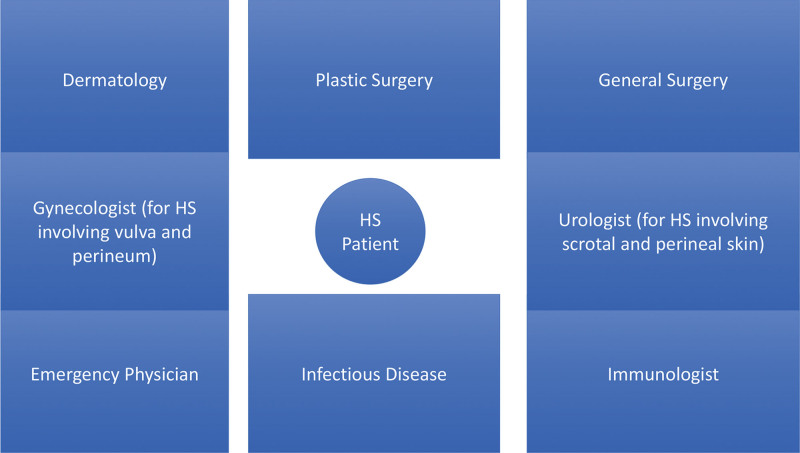
- Multidisciplinary care: Principally dermatology is the “home” for HS patients, and plastic surgeons, internists, infectious disease specialists, and immunologists provide “multidisciplinary care,” an ideal HS service-line model15 (Fig. 3).
- Demand: HS has a devastating effect on patients (most of whom are young, minorities, and underserved): poor quality of life,16 chronic pain,17 poor mental health,18 substance abuse,19 impaired intimate relationships,20 with two to four times higher suicide rates than the general population.21 Understandably, these patients deserve a lasting, resolute, durable, and definitive treatment, instead of multiple lifelong treatments that cycle between remissions and flare-ups.
DESCRIPTION OF MOST EFFECTIVE PROCEDURES
Broadly, selection of the surgical operation depends upon two criteria:
- Disease acuity:
- Hurley stage:
- ○Limited disease: Solitary lesions can be treated with local excision, deroofing, and skin-tissue-sparing excision with electrosurgical peeling (STEEP).24 STEEP involves successive tangential excisions of lesional and fibrous tissue until the epithelialized bottom of the sinus tracts is reached, and left open to heal secondarily. This tissue-sparing technique has low recurrence rates and high patient satisfaction with relatively short healing times and favorable cosmetic outcomes.
- ○Severe widespread disease: it needs an extensive resection (wide or radical excision, described in detail below), including resection of chronic inactive lesions that are harbingers of recurrence.25




Leave a Reply